A Facet of My Life in Block 4.2
Saturday, 29 January 2011
2011 announcement
Saturday, 4 December 2010
AIDS at a glance…
Acquired Immune Deficiency Syndrome (AIDS)
In conjunction with the World AIDS Day on December 1st that was three days ago, I would like to dedicate a post to this blog to raise awareness of the AIDS pandemic caused by the spread of HIV infection. I am sure many of you know what AIDS is and what HIV is. So I would like to skip the medical and science part and go straight to the awareness and theme of AIDS.
This year, the theme of World AIDS Day is “Universal Access and Human Rights”. World AIDS Day is important for reminding people that HIV has not disappeared and that there are still many things to be done.
AIDS is now pandemic. According to UNAIDS estimates, there are now 33.3 million people living with HIV, including 2.5 million children. During 2009 some 2.6 million people became newly infected with the virus and an estimated 1.8 million people died from AIDS.
Global leaders have pledged to work towards universal access to HIV and AIDS treatment, prevention and care, recognising these as fundamental human rights. Significant progress has been made in increasing access to HIV and AIDS services, in spite of that greater commitment is still needed around the world if the goal of universal access is to be achieved.

Millions of people continue to be infected with HIV every year. In low- and middle-income countries, less than half of those in need of antiretroviral therapy are receiving it, and too many do not have access to adequate care services.

The protection of human rights is fundamental to combating the global HIV and AIDS epidemic. Violations against human rights fuel the spread of HIV, putting marginalised groups, such as injecting drug users and sex workers, at a higher risk of HIV infection. By promoting individual human rights, new infections can be prevented and people who have HIV can live free from discrimination and social stigmatism.
World AIDS Day provides an opportunity for all of us - individuals, communities and political leaders - to take action and ensure that human rights are protected and global targets for HIV/AIDS prevention, treatment and care are met.
Therefore, we should start by wearing a red ribbon to promote AIDS awareness and if possible educate the people about the epidemic itself. Besides that, by wearing the red ribbon, we demonstrate care and concern about HIV and AIDS, and to remind others of the need for their support and commitment.

You could also take your awareness raising a step further by trying to find a local event to take part in. Around the world there are hundreds of activities taking place to mark World AIDS Day, including candlelight vigils, art shows, marches and religious services. If you can't find anything in your area then why not organise an event yourself? When there’s a will, there’s a way. Hehe.
There is an organization called AVERT which has AIDS projects in the parts of the world most severely affected by HIV and AIDS. They are helping the people there deal with their challenges such as extreme poverty, stigma and lack of healthcare by providing them education, treatment and care. The projects also help the orphaned children or otherwise affected by HIV and AIDS.
So maybe you could lend a hand in the fundraising program to help AVERT or maybe donation or sponsorship in helping those who are suffering from the outcome of AIDS.
Lastly, I would like to quote a phrase from my friend, where I would like this phrase to be the ending of my post. “To Care Is To Give”
References:
http://en.wikipedia.org/wiki/AIDS
http://en.wikipedia.org/wiki/World_AIDS_Day
Friday, 3 December 2010
CDM2
Comprehensive Disaster Management 2
From the previous post, I mentioned about the 6 main components of the conceptual framework of disaster. In this post, the actions that are derived from the main components like what is their definition, function and description will be discussed and I welcome anyone who would want to post any comment or suggestion on my post. Thank you.
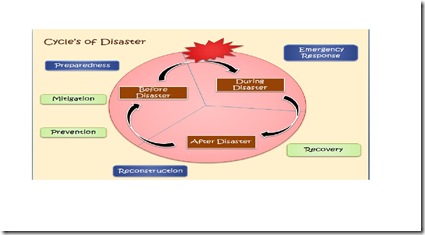
In disaster management, there are 3 phases that forms the framework, which is the pre-disaster phase, during disaster and post-disaster phase. And in these phases the actions derived from the 6 main components of the framework will play their function in disaster managing. The actions are prevention, preparedness, mitigation, resilience, response and recovery.
In prevention, we try to avoid or minimize the hazard. For example, we can do an evacuation. Otherwise, we could also try to prevent the hazard from turning into a disaster by doing selective preventive measures that are useful and effective.
For preparedness, it is a continuous cycle of planning, organizing, training, equipping, exercising, evaluating, improvement activities, and increasing capabilities to prevent, protect against, respond, recover, and mitigate effects of disasters. The actions are preparing a good communication system, preparing the response team, preparing shelter or evacuation plan, stockpiling supplies, trained volunteers (Red Cross, MERCY) and lastly give warnings to the society about the condition of the hazard. In preparedness, casualty prediction is required to anticipate the worst come to worst outcome of the hazard.
As for mitigation, it is defined as an action to lessen or reduce the force or impact of the hazard. The principles of mitigation are to prevent hazard to turn into disaster, reduce the effect of disaster when it occur, and focus on long term measures in reducing or eliminating risk. Mitigation is classified into structural and non-structural measures. Structural mitigation is an engineering measure that deals with the resistance and resilience of the infrastructures, houses, and facilities in reducing the impact of disaster. To increase the ability to face the disaster, non-structural mitigation deals with the awareness of the community, policies from the government and warning system to the community.
In response, there is the mobilization of emergency services and the first responders are to set up an incident command system to coordinate and communicate with other responders. There are many parties that played a role in this action, which are firefighters, police, ambulance, rapid response team, search & rescue team as well as the military soldiers. When this response is conducted as military operation, it is call a disaster relief operation. Vast majority of individuals will die within 72 hours of impact therefore it is of most importance that the victims are to be found within that stated time.
In recovery, there are two sub-actions which are the rehabilitation and the reconstruction. Disaster recovery is the process, policies and procedures related to preparing for recovery or continuation of technology infrastructure critical to an organization after a natural or human induced disaster. Rehabilitation focuses on the improvement and restoration of all aspects of public services and the normalization or the progression of daily life of the affected people. In reconstruction, the redevelopment or development of all infrastructures and facilities are being done to make sure the community affected can regain their daily routine as soon as possible. The recovery process is important so that the community can function properly in order to progress economically, socially, and culturally.
References:
Lecture Notes Block 4.2 (Conceptual Framework of Disaster and Disaster Management, Logistic Management Support, and Preparedness, Response, and Recovery)
A Comprehensive Conceptual Model for Disaster Management
Sohail Asghar, Damminda Alahakoon and Leonid Churilov
Clayton School of Information Technology, Monash University, Australia
Thursday, 2 December 2010
CDM
Comprehensive Disaster Management
Ever wonder which government organization is responsible for the management of disaster should a catastrophic event occurred? Or else, instead the private or NGO corporation are the ones who are responsible when there is a calamity? Actually, the body or structure that is responsible for disaster management is known as the CRC, crisis response centre.
This centre is responsible for the management of disaster either man-made or natural. Also, they are the ones who are in charge during the process. They have to coordinate and manage the flow of aid internally and externally. Internal aids are those involved in the fieldwork. For example, the search & rescue teams, medical doctors who are specialize in emergency and disaster medicine, nurses, rescue volunteers, soldiers, paramedics, and many more. As for the external aid, the examples are the NGOs, the central government, the private companies or sectors, and multilateral agencies as well as other organizations.
In Jogjakarta, the crisis response centre in charge is known as the BNPB, Badan nasional Penaggulangan Bencana. They will command the local government (BPBK/KT) and the governor (BPBP) coordinate and cooperate with them in handling their respective districts and regions. Besides that, the BNPB will collaborate with the district health office and the provincial office in aiding the refugees and victims of the disaster. Monetary funding will be provided from the Ministry of Health where the revenue will be relayed to the BNPB for purchasing the resources needed to support the refugees.

The resources are listed in the following:
· medicines
· health supplies / kits
· water and environmental health
· food
· logistic / administration
· shelter-electrical-construction
· personal needs / education
· human resources
· agriculture / livestock
· unclassified / others
Basically, the main thing to handle or manage a disaster is to follow the disaster conceptual framework which has 6 main components. The components are hazard, risk, events, impact, damage and disaster. From there, we can develop a few actions that composed of prevention, preparedness, mitigation, resilience and recovery development to help in the management of the disaster.

Hazard is the physical effects generated in the naturally occurring event. Another definition is a dangerous condition or events that threatens or have the potential for causing injury to life or damage to property or the environment.
Risk is defined as a measure of the expected losses (deaths, injuries, property, economic activity etc) due to hazard of a particular magnitude occurring in a given area over a specific time period.
Event is the realization of hazard. Impact is the contact between an event and society. Damage is the negative result from the impact of an event. After damage, there would be a change of social function where if there is a need of external aid for recovery then it is called a disaster. If there is no external aid needed then it is just an event.
Here I discussed about the 6 main components of the framework and its definitions and as for their respective actions, I will discuss it at my next post. So stay connected with my next post. Lastly, I would like to conclude that practice makes perfect therefore it is better to do the planning, prevention, mitigation and also the management before the disaster happen so that to provide the best service and support to those who require them.
References:
Lecture Notes Block 4.2 (Conceptual Framework of Disaster and Disaster Management, Logistic Management Support, and Preparedness, Response, and Recovery)
Sunday, 28 November 2010
A Model that Benefits the Chronic Patients

Chronic Care Model
Model Elements
The Chronic Care Model (CCM) recognizes the essential elements of a health care system that encourage high-quality chronic disease care. These elements are the community, the health system, self-management support, delivery system design, decision support and clinical information systems. Evidence-based change theories under each element, in turn, foster productive interactions between informed patients who take an active part in their care and providers with resources and expertise.
The Model can be applied to a variety of chronic illnesses, health care settings and target populations. The bottom line is healthier patients, more satisfied providers, and cost savings.
Dr Wagner developed the chronic care model and his collaborates helped in the development as well as the refinement of the model. Further information can be found in this link I have provided: http://www.improvingchroniccare.org/index.php?p=Model_Elements&s=18
Promoting effective change in provider groups to support evidence-based clinical and quality improvement across a wide variety of health care settings.
From many surveillance data collected over the past years, we can see that many chronic diseases has emerged in the population and Almost half of all people with chronic illness have multiple conditions. As a result, many managed care and integrated delivery systems have taken a great interest in correcting the many deficiencies in current management of diseases such as diabetes, heart disease, depression, asthma and others.
Those deficiencies include:
- Rushed practitioners not following established practice guidelines
- Lack of care coordination
- Lack of active follow-up to ensure the best outcomes
- Patients inadequately trained to manage their illnesses
To overcome the deficiencies, it will require the transformation of health care, from a system that is essentially reactive, responding mainly when an individual is sick, to one that is proactive and focused on keeping an individual as healthy as possible. Thus, to accelerate the transition, Improving Chronic Illness Care (ICIC) created the Chronic Care Model (CCM), which summarizes the fundamental elements for improving care in health systems at the community, organization, practice and patient levels.
The CCM consists of two main components, which is the health system and the community. Each of the components contains a few of the fundamental elements.
The model suggests that the patient-provider interactions resulting in care that improves outcomes are found in health systems that:
· have well-developed processes and incentives for making changes in the care delivery system
· assure behaviourally sophisticated self-management support that gives priority to increasing patients' confidence and skills so that they can be the ultimate manager of their illness.
· reorganize team function and practice systems (e.g., appointments and follow-up) to meet the needs of chronically ill patients
· develop and implement evidence-based guidelines and support those guidelines through provider education, reminders, and increased interaction between generalists and specialists
· enhance information systems to facilitate the development of disease registries, tracking systems, and reminders and to give feedback on performance.
Health system
Delivery System Design
Assure the delivery of effective, efficient clinical care and self-management support
- Define roles and distribute tasks among team members
- Use planned interactions to support evidence-based care
- Provide clinical case management services for complex patients
- Ensure regular follow-up by the care team
- Give care that patients understand and that fits with their cultural background
Clinical Information Systems
Organize patient and population data to facilitate efficient and effective care
- Provide timely reminders for providers and patients
- Identify relevant subpopulations for proactive care
- Facilitate individual patient care planning
- Share information with patients and providers to coordinate care
- Monitor performance of practice team and care system
Decision Support
Promote clinical care that is consistent with scientific evidence and patient preferences
- Embed evidence-based guidelines into daily clinical practice
- Share evidence-based guidelines and information with patients to encourage their participation
- Use proven provider education methods
- Integrate specialist expertise and primary care
Community
Resources and Policies
Mobilize community resources to meet needs of patients
- Encourage patients to participate in effective community programs
- Form partnerships with community organizations to support and develop interventions that fill gaps in needed services
- Advocate for policies to improve patient care
Self-Management Support
Empower and prepare patients to manage their health and health care
- Emphasize the patient's central role in managing their health
- Use effective self-management support strategies that include assessment, goal-setting, action planning, problem-solving and follow-up
- Organize internal and community resources to provide ongoing self-management support to patients
By focusing on the improvement of those 5 elements, the individuals whom are suffering from chronic diseases will be treated, managed, and received the medical attention needed in order for them to live life productively without complications and deterioration of their disease condition.
References:
http://www.acponline.org/clinical_information/journals_publications/ecp/augsep98/cdm.htm
http://www.improvingchroniccare.org/index.php?p=The_Chronic_Care_Model&s=2
Thursday, 25 November 2010
CDM? CCM?
Chronic Disease Management (CDM)
As I was preparing for my Week 4 tutorial, I came across something intriguing that I would like to share it to those who read my blog on health system. The interesting yet intriguing read was about chronic care management.
What is chronic care management? What is chronic disease management?
Let’s begin by understanding the term chronic disease. Firstly, chronic diseases are prolonged conditions that often do not improve and are rarely cured completely. Diabetes, depression, congestive heart failure, hepatitis and asthma are examples of chronic diseases. Approximately 1 in 4 British Columbians have benn diagnosed with one or more chronic diseases.
Chronic illness has a profound effect on the physical, emotional and mental well-being of individuals suffering from it, often making it difficult to carry on with daily routines and relationships. However, in many cases, deterioration in health can be minimized by good care. This often depends upon individual choices made on a daily basis as well as the collaboration of the physicians in charge as well.
Chronic care management encompasses the oversight and education activities conducted by professionals to help patients with chronic diseases such as diabetes, high blood pressure, lupus, multiple sclerosis and sleep apnea learn to understand their condition and live productively with it. This term is equivalent to disease management (health) for chronic conditions, i.e. Chronic Disease Management. The effort involves motivating patients to persist in necessary therapies and interventions and helping them to achieve an ongoing, reasonable quality of life.
Chronic disease management (CDM) is a systematic approach to improving health care for people with chronic disease. Health care can be delivered more effectively and efficiently if patients with chronic diseases take an active role in their own care and providers are supported with the necessary resources and expertise to better assist their patients in managing their illness.
So, may I ask why CCM/CDM emerges or surfaces into the medical health system? This is because usual care is not doing the job; dozens of surveys and audits have revealed that sizable proportions of chronically ill patients are not receiving effective therapy, have poor disease control, and are unhappy with their care.
Although acute care has characterized all medical care until recently, several varieties of managed care have emerged in the past decades in an effort to improve care, reduce unnecessary service utilization and control spiraling costs. Despite its initial promise, however, managed care has not achieved truly coordinated care. In actual operation it appears to emphasize its fiscal goals. Moreover, managed care does not address the complexity of chronic conditions, and in the interests of cost-cutting, tends to reduce time with patients rather than increase it.
Well, Dr. Wagner has his own opinion on the matter. He believes that if we are to improve care for most patients with chronic illness, the evidence strongly suggests that we reshape our ambulatory care systems for this purpose. Primary care practice was largely designed to provide:
- ready access and care to patients with acute, varied problems,
- with an emphasis on triage and patient flow;
- short appointments;
- diagnosis and treatment of symptoms and signs;
- reliance on laboratory investigations and prescriptions;
- brief, didactic patient education; and
- patient-initiated follow-up.
Patients and families struggling with chronic illness have different needs, and these needs are unlikely to be met by an acute care organization and culture. They require:
- planned, regular interactions with their caregivers,
- with a focus on function and prevention of exacerbations and complications.
This interaction includes:
- systematic assessments,
- attention to treatment guidelines, and behaviourally sophisticated support for the patient's role as self-manager.
- education to the patient on the benefits of treatment and the risks of not properly following their treatment regimen.
- patients need to be motivated to comply because treatment usually produces an improved state, rather than the results that most patients desire -- a cure.
These interactions must be linked through time by clinically relevant information systems and continuing follow-up initiated by the medical practice.
In the next post, I would like to emphasize on the elaboration of a chronic care model developed by Dr. Wagner and his collaborators, its standards and guidelines, importance, structure as well as its components. Tune in to my next post as it will reveal the solution for tackling the problems that occurred in the current acute-care model of care delivery.
References:
Wagner, E.H. Chronic disease management: What will it take to improve care for chronic illness? Effective Clinical Practice. 1998;1:2-4.
Ware, N.C., et al. (2000). Clinician experiences of managed mental health care: A rereading of the threat. Medical Anthropology Quarterly, 14(1), 2-27.
Wagner EH. Managed care and chronic illness: health services research needs. Health Serv Res. 1997;32:702-14.
http://en.wikipedia.org/wiki/Chronic_care_management
http://www.acponline.org/clinical_information/journals_publications/ecp/augsep98/cdm.htm
Monday, 22 November 2010
The Role of PHC in Developing Countries
PHC
After having an interesting and interactive discussion during a Week 4 tutorial session with my group mates, I am spurred by my strong motivation and interest to share the content of discussion about PHC in our tutorial seesion.
First of all, What is PHC? What does this medical abbreviation mean?! Ok, I will let you know right here, right now. PHC stands for Primary Health Centre. It is in accordance with the Alma Ata Declaration, 1978 by the member nations of WHO; in which PHCs were established to provide accessible, affordable and available primary health care to people.
The Declaration of Alma-Ata was adopted at the International Conference on Primary Health Care(PHC), Almaty (formerly Alma-Ata), currently in Kazakhstan, 6-12 September 1978.[1]It expressed the need for urgent action by all governments, all health and development workers, and the world community to protect and promote the health of all the people of the world. It was the first international declaration underlining the importance of primary health care. The primary health care approach has since then been accepted by member countries of WHO as the key to achieving the goal of "Health for All".
In South Asia, PHCs are the basic structural and functional unit of the public health services in developing countries. They are the cornerstone of rural healthcare where in these rural places, health services and healthcares are scarce. Therefore the establishment of PHCs and their sub-centres in rural areas are to meet the health care needs of rural population.
Objectives of PHC are organizing health efforts that are comprehensive, integrated, equitable, acceptable and affordable by the community, with active participation of the community and use the results of science and appropriate technology, a cost that can be carried by government and society. Health effort was organized by focusing on service to the wider community in order to achieve optimal health degree, without sacrificing quality of service to individuals. Lastly, they should provide preventive, promotive, and curative to rehabilitative either through the efforts of individual health (UKP) or public health efforts (SME).
Each primary health centre covers a population of 1,00,000 and spread over about 100 villages. Other sources, said that theoretically every 30,000 population gets one PHC. Each PHC has five or six sub-centres staffed by health workers for outreach services such as immunization, basic curative care services and maternal and child health services. PHCs generally consist of one or more doctors, a pharmacist, staff nurse and other paramedical support staff.
Below are the job scopes of a PHC:
- Medical care.
- Mother and child health care including family planning.
- Safe water supply and basic sanitation.
- Prevention and control of local diseases.
- Collecting statistical information.
- Health education.
- Training of health guides, health workers, dayees.
- Basic laboratory investigations.
In Indonesia, Puskesmas (Pusat Kesehatan Masyarakat) is the PHC that is located at the rural areas of the country. Puskesmas provides in-patient and out-patient services that were agreed by the health centres and health authorities concerned. In providing services in the community, puskesmas usually has a subunit of services such as health centres (puskesmas pembantu), mobile health clinic (puskesmas keliling), neighborhood health center (posyandu), rural health post (pos kesehatan desa) and village maternity posts (polindes).
In India, PHC's form a basic part of the health care system. The Medical Officer who provide services through the PHC's must be a MBBS degree holder. In addition to the provision of diagnostic and curative services, the Medical Officer also acts as the primary administrator for the PHC.
The primary field staff, who provide outreach services, are called "ASHA (Accredited Social Health Activist)" or village health nurse, depending upon the Indian state where the PHC is located. The village health nurse provides service at the point care, often in the patient's home. If additional diagnostic testing, or clinical interventions were required, the patient would be transported to the PHC to be evaluated by the Medical Officer.
Now under national rural health mission PHC are rapidly upgraded. Therefore, there are many health services that can be provided by puskesmas or PHC which includes an ECG (electrocardiogram), minor surgery, neonatal resuscitation, implants, nebulizers, maternal ward and some also have X-rays as well as a defibrillator.
Recently, a selective primary health care (PHC) approach referred to collectively under the acronym GOBI-FFF, these are strategies that are being adopted to improve maternal and child health as part of primary care. GOBI-FFF is a model of a PHC. Respectively they include:
- Growth monitoring
- Oral rehydration therapy
- Breast-feeding
- Immunization
- Family Spacing (planning)
- Female Education
- Food Supplementation
This was further reduced to GOBI only (selective PHC) on the priorities set by donors for poor countries.
References:
www.wikipedia.com (keyword: primary health centre, community health centre, Alma Ata Declaration, Puskesmas)
india.gov.in (keyword: primary health centre)